To go further
- “These sexist biases that threaten women’s health” — Article written by Anne Guion, La Vie (2023):
- “These medical diagnoses biased by gender stereotypes” — Article written by Solenn Cordroc’h, Slate (2021)
- “Gender bias in clinical trials puts women at risk” — Article written by Marcus Dupont-Besnard, Numerama (2020)
- When medications threaten women’s health — Article written by Andréane Williams, La Gazette des Femmes (2016)
- “Women and health, still a men’s affair?” -Book co-written by Catherine Vidal and Muriel Salle (2017) andPodcastwith Catherine Vidal (2020).
- “The inclusion of women in clinical trials : Are we asking the right questions” -PDF par Abby Lippman (2006).
Sources
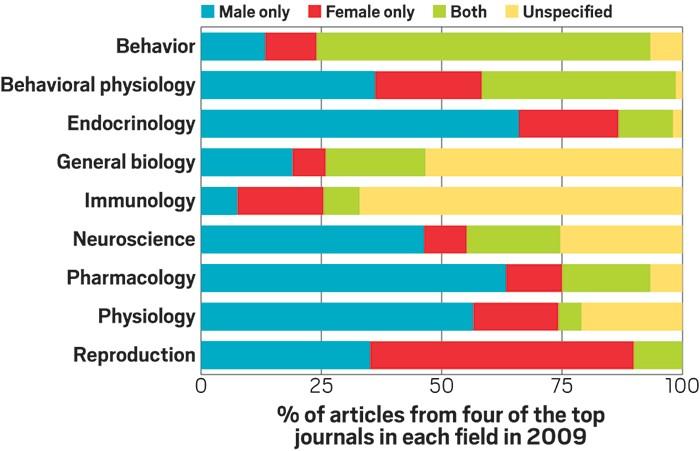
[1] « Are biomedical researchers forgetting females ? », Chemical & Engineering News. Consulté le : 6 mars 2024. [En ligne]. Disponible sur : https://cen.acs.org/articles/95/i12/biomedical-researchers-forgetting-females.html
[2] L. M. Harrison, D. W. A. Noble, et M. D. Jennions, « A meta-analysis of sex differences in animal personality : no evidence for the greater male variability hypothesis », Biol. Rev. Camb. Philos. Soc., vol. 97, no 2, p. 679‑707, avr. 2022, doi : 10.1111/brv.12818.
[3] A. K. Beery et I. Zucker, « Sex bias in neuroscience and biomedical research », Neurosci. Biobehav. Rev., vol. 35, no 3, p. 565‑572, janv. 2011, doi : 10.1016/j.neubiorev.2010.07.002.
[4] I. Zucker et B. J. Prendergast, « Sex differences in pharmacokinetics predict adverse drug reactions in women », Biol. Sex Differ., vol. 11, no 1, p. 32, juin 2020, doi : 10.1186/s13293-020 – 00308‑5.
[5] F. Butlen-Ducuing et al., « Implications of sex-related differences in central nervous system disorders for drug research and development », Nat. Rev. Drug Discov., vol. 20, no 12, p. 881‑882, déc. 2021, doi : 10.1038/d41573-021 – 00115‑6.
[6] I. of M. (US) F. on N. and N. S. Disorders, « Studying Sex Differences in Health and Disease », in Sex Differences and Implications for Translational Neuroscience Research : Workshop Summary, National Academies Press (US), 2011. Consulté le : 6 mars 2024. [En ligne]. Disponible sur : https://www.ncbi.nlm.nih.gov/books/NBK53393/
[7] N. R. Osborne et K. D. Davis, « Sex and gender differences in pain », Int. Rev. Neurobiol., vol. 164, p. 277‑307, 2022, doi : 10.1016/bs.irn.2022.06.013.
[8] T. Keteepe-Arachi et S. Sharma, « Cardiovascular Disease in Women : Understanding Symptoms and Risk Factors », Eur. Cardiol. Rev., vol. 12, no 1, p. 10‑13, août 2017, doi : 10.15420/ecr.2016:32:1.
[9] C.-S. M. Center, « A decade of women’s heart health, reexamined ». Consulté le : 7 mars 2024. [En ligne]. Disponible sur : https://medicalxpress.com/news/2022 – 02-decade-women-heart-health-reexamined.html
[10] « The Principles of Humane Experimental Technique », Med. J. Aust., vol. 1, no 13, p. 500‑500, 1960, doi : 10.5694/j.1326 – 5377.1960.tb73127.x.
[11] C. E. Krebs et al., « Author Guide for Addressing Animal Methods Bias in Publishing », Adv. Sci. Weinh. Baden-Wurtt. Ger., vol. 10, no 30, p. e2303226, oct. 2023, doi : 10.1002/advs.202303226.
[12] A. Duchesne, C. Tannenbaum, et G. Einstein, « Funding agency mechanisms to increase sex and gender analysis », Lancet Lond. Engl., vol. 389, no 10070, p. 699, févr. 2017, doi : 10.1016/S0140-6736(17)30343 – 4.
[13] I. Miguel-Aliaga, « Let’s talk about (biological) sex », Nat. Rev. Mol. Cell Biol., vol. 23, no 4, p. 227‑228, avr. 2022, doi : 10.1038/s41580-022 – 00467‑w.
[14] M. M. Reid et al., « Demographic diversity of US-based participants in GSK-sponsored interventional clinical trials », Clin. Trials, vol. 20, no 2, p. 133‑144, avr. 2023, doi : 10.1177/17407745221149118.